What We Learn from a Negative Study: Pork Production and Public Health
Last month, the Journal of Agricultural and Food Chemistry published a study about the authors’ search for the residue of a known human carcinogen in off-the-shelf pork products. Contrary to what they expected, the researchers, several of whom are affiliated with the Johns Hopkins Center for a Livable Future and the Prasse Lab at the Bloomberg School (BSPH), did not, in fact, find any residue of the known human carcinogen. If the result was surprising or confusing, it was, at least, good news for people who eat those particular pork products. And the research led to the development of what seems like a new and better way to test for the residue—one that the FDA would be wise to consider adopting.
The Carbadox Impasse
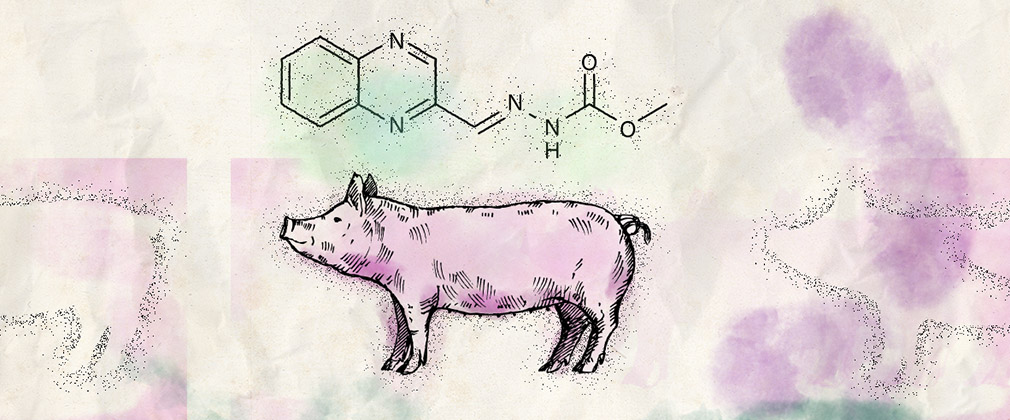
The carcinogen in question is a veterinary drug known as carbadox, an antibiotic. Some industrial livestock producers feed it to their piglets to control diseases and promote weight gain. When the drug is fed to pigs, it breaks down inside the animal’s body into smaller chemicals—metabolites—that can remain in the edible pork tissue after the pig is slaughtered, and some of these metabolites are known to cause cancer in humans.
Two years ago (November, 2023), the Federal Drug Administration (FDA) proposed a ban on carbadox, which was promptly opposed by the manufacturer of carbadox. A long legal battle is in process, and the drug is still legal and available for use in swine at this point.
The drug was approved for use in animals first in 1972 and then again in 1998. Matthew Newmeyer, an analytical chemist in the Prasse Lab, a research associate at BSPH, and a co-author of the study, explained the carbadox impasse as “a weird, legal purgatory.” Two of the metabolites that result from carbadox and can show up in pork products are QCX and desoxycarbadox. Desoxycarbadox is a human carcinogen, and QCX is not. But—and here’s the tricky part—it’s been difficult historically to measure for desoxycarbadox.
Because of this challenge, the FDA has allowed measuring for QCX and using it as a proxy, or surrogate, to indicate the presence of desoxycarbadox, the carcinogen.
But in 2003, new data became available, showing that desoxycarbadox persisted in pork tissue longer than QCX did, which made QCX a less reliable surrogate. As a result, the Joint FAO/WHO Expert Committee on Food Additives decided that we can no longer use QCA to measure for the presence of the carcinogen desoxycarbadox. And for its own reasons, the FDA decided to stick with measuring QCA.
“The FDA is essentially using a chemical that we know is not an appropriate surrogate for the thing we care about,” says Newmeyer.
A Doctoral Fellow Gets Introduced to Food Systems Transparency Issues
Last month’s study showed a “negative result” for both QCA and desoxycarbadox in pork products they purchased at grocery stores. Newmeyer refers to the study’s findings as a “negative result,” taking care to emphasize that the term means different things to different people. As a chemist, he uses the term only to denote that they didn’t detect any residue.
For co-author Mei-Li Hey, a CLF-Lerner Fellow and doctoral student, the negative result was confusing.
“We didn’t know how to interpret the fact that we didn’t detect any residue in the samples,” she says. “It could be that the pigs were never fed carbadox. Or it could be that the pigs were fed carbadox, but enough time elapsed for the metabolites to disappear.”
“Mei-Li spent a lot of time inventorying the products that we used in the study,” says Newmeyer. “We had many meetings about how many of these products we were going to choose, and it’s a strength of our study.”
Hey investigated more than 600 pork products sold in 10 Baltimore County and Baltimore City stores, taking photos and cataloguing them with regard to processing, cooking, and flavoring—all in search of pork products that were minimally processed or interfered with. They looked at bacon, scrapple, pork shoulder, and pork butt. Hey says they were looking for as pure a piece of meat as they could get, and she wanted as much information as she could get on each sample.
She decided to call the pork producers and ask them if they used carbadox in their production of the pigs.
“I thought they might tell us if they used carbadox,” she says. “I was optimistic in the beginning, thinking why wouldn’t they tell us what they used?”
Keeve Nachman, the senior author on the study, approved this course of action.
Hey recalls, “Keeve was like, ‘All right, go ahead and call them.’ And there was only one conversation that I had that I would characterize as good or productive.”
Hey reached out to integrators using email, phone calls, and online contact forms, and only once was she connected to a veterinarian who would answer her questions. She contacted 13 integrators, and 12 of then either failed to respond or brushed her off (see Table 3, below). One integrator told her that they only used carbadox to treat dysentery.
“This speaks to the importance of negative results,” says Hey. “It’s important to report when there’s no information, because it actually gives you some information. If no one responds, that tells us that the system is opaque.”
The Research Teams Uses a Novel Approach for Measuring Carbadox Residues
Newmeyer explains that QCA and desoxycarbadox are very different chemically, and for that reason, it’s difficult to test for both in the same method. And because the non-carcignogenic marker residue QCA has been historically easier to measure than the carcinogenic metabolite desoxycarbadox, the easier path is to look for the non-carcinogenic QCA alone. If you want to test for the actual carcinogen—desoxycarbadox—you’ll need to test for both metabolites, and that would be a more difficult path, requiring the scientists to conduct two entirely separate sets of testing with the same sample. Newmeyer wanted to make it simpler.
“We wanted to take one sample and do one isolation and analysis method to measure for both,” says Newmeyer. “And we wanted to maintain the same level of sensitivity. So, yes, we did develop a new method.”
A significant part of the study is a discussion about these different, novel methods.
This particular study of 30 samples showed residue for neither QCX nor desoxycarbadox—an interesting result in itself—but the fact that it’s now so much easier to test for both is positive momentum.
“If the ultimate decision by FDA is to continue allowing carbadox,” says Newmeyer, “I hope they’ll use our method. Or even just use it to test for desoxycarbadox alone. They can adapt the method as needed.”
“While carbadox is still in use, there need to be further studies,” says Hey.
An avenue of research that appeals to both Hey and Newmeyer is the period of time that it takes for a pig’s body to eliminate carbadox. The current thinking is that it takes 42 days.
“The most important thing for any of those studies is to use the most sensitive method available to measure for desoxycarbadox, because that’s a carcinogen we don’t want in any of our food. We need to know how long it’s detectable using the most sensitive method available.”
Hey is pleased that their study is reporting the “negative result.” For this study, she says, not finding a carcinogen in pork is a positive thing for public health. And reporting their work, whether or not the findings validate the researchers' hypothesis, is a big step in supporting transparency in food systems research.
“Transparency is always going to be really important. I’m an implementation scientist, and there are a lot of instances in research when finding what didn’t go well is difficult but would be super helpful. Just report the results you get, so somebody doesn’t try this again. This time it was a good thing that we didn’t find anything.”
Table 3. Responses Regarding Carbadox Use among Pork Integrators Whose Products Were Tested
| Integrator No. | Response Characterization | Detailed Response (if applicable) |
|---|---|---|
| 1 | No response | |
| 2 | No response | |
| 3 | CBX not used | No policies in place about the use of carbadox by pork farmers; the pork purchased is “raised without antibiotics.” |
| 4 | No response | |
| 5 | Unknown based on response | Some antibiotics are used, but cannot guarantee that carbadox is not used. |
| 6 | No response | |
| 7 | No response | |
| 8 | Unknown based on response | Indicated that no policies in place about the use of carbadox by pork farmers could be found at this time. |
| 9 | No response | |
| 10 | No response | |
| 11 | CBX is used | CBX used only to prevent and treat dysentery. |
| 12 | Unknown based on response | Indicated they cannot release any information on antibiotic use to the public. |
| 13 | Unknown based on response | Indicated they do not sell pork. |
Banner image: Mike Milli, 2025