Gauging Federal Support for Veggie Scripts
BALTIMORE—April 15, 2020. An apple a day keeps the doctor away. We all know that fresh fruits and veggies are an important part of a healthy diet, and public health practitioners agree —but actually getting people to eat fruits and vegetables is a whole different challenge. There are, however, a great variety of interventions aimed at increasing fruit and vegetable consumption throughout the United States and beyond.
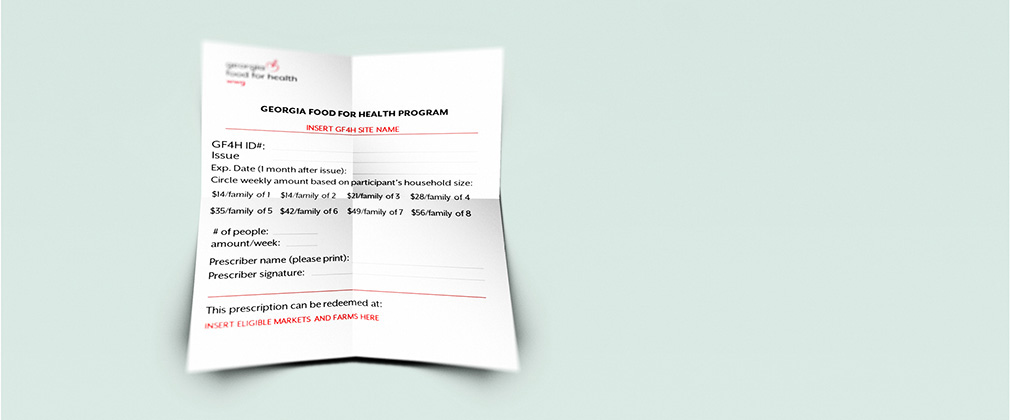
“Veggie scripts,” or “veggie Rx,” have emerged in recent years as one such intervention. These produce prescription programs are practical public health interventions that aim to increase fruit and vegetable consumption, and also reduce food insecurity and decrease health care costs. In these programs, health care professionals write patients a “prescription” for fruits and vegetables, and the patient redeems the prescription at a nearby farmers market or grocery store, usually at no cost or at a discounted price.
While pursuing my Masters in Public Health at the Johns Hopkins Bloomberg School of Public Health, I wanted to learn about how policy might support healthy food systems while also promoting public health, local economies, and environmental sustainability. Because produce prescriptions appear to be a powerful tool for improving public health and supporting local farmers, I wanted to know if there was any interest at the federal level to support these programs. Produce prescription programs have been in existence for 15 years, but have not been explicitly included in federal policy. So it was a natural fit for me to learn more about how veggie scripts got onto the agenda of federal policymakers and how funding for it came to be included in the 2018 Farm Bill. The result of my investigation is a new Johns Hopkins Center for a Livable Future report, “Veggie Rx in the 2018 Farm Bill.”
In the report, I explore what happened between 2002 and 2018 to bring the program to fruition. One of my findings is that the concept of dedicating federal funding to support such a program stems from the healthy eating incentive programs that were first proposed in the 2002 Farm Bill. In December, 2018, President Trump signed the 2018 Farm Bill, which included dedicated federal funds for produce prescription programs for the first time ever in the United States. These funds were incorporated as part of the Gus Schumacher Nutrition Incentives Program (GusNIP), formerly known as the Food Insecurity Nutrition Incentives (FINI) program.
Through my interviews with several nonprofits and Congressional staff members involved in including produce prescriptions in the 2018 Farm Bill, it became clear that some have a long-term vision for the future of produce prescriptions to be embedded in the fabric of the American health care system. Imagine a future in which Medicare or Medicaid reimburses doctors nationwide for prescribing fruits and vegetables to millions of patients across the United States! Like many policies, the finances are likely to determine whether or not this vision can become a reality.
The evaluation of this latest round of Farm Bill funding should help determine the potential health care savings if produce prescriptions were implemented on a larger scale.
Perhaps in the future, an apple (and some spinach and sweet potatoes) a day will not only keep the doctor away, but also reduce the health care costs associated with diet-related chronic disease.
Emily Hennessee is a graduate of the Master of Public Health program at the Johns Hopkins Bloomberg School of Public Health with a concentration in food systems and certificates in public health advocacy and health communications.
Image: Original artwork by Michael Milli, 2020.